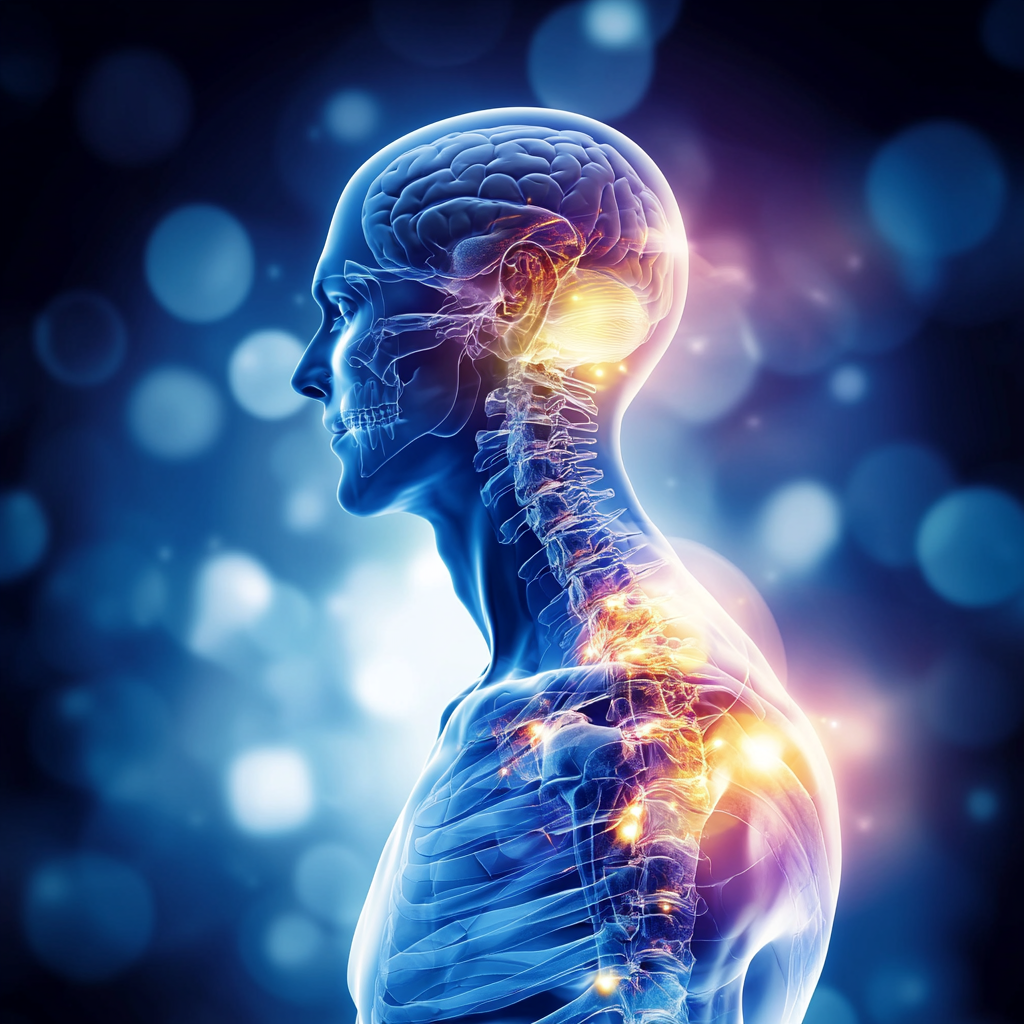
The Glaring Omission of the Endocannabinoid System From Medicine

While it is a major regulator of human physiology, the endocannabinoid system (ECS) is still excluded from the traditional medical school curriculum.
Dr. Stefan Broselid, a medical pharmacologist, attributes the blame for misunderstandings and suboptimal utilization of medical cannabis on a lack of knowledge among doctors.
In a 2022 UK report, nearly 40,000 practitioners were licensed to prescribe medical cannabis, yet less than 100 do, with the knowledge gap being apparent.
The ECS is a sophisticated control mechanism which influences a vast number of varied body functions, including mood, pain, appetite, memory, and immune function.
Its non-inclusion in medical school curricula is a critical learning deficiency that compromises patient care. Dr. Broselid endorses including ECS education in medical school curricula, mentioning that education on such a type of system is essential for overall patient care.
The implications of this knowledge gap are wider than prescribing.
Clinicians who are not ECS-knowledgeable might be hesitant to talk to patients about cannabis medicines, which could restrict therapeutic potential across a spectrum of conditions from pain, which is frequently chronic, to epilepsy.
Furthermore, a lack of education is preventing evidence-based conversations about using cannabis, with the patient being left without appropriate medical advice on what treatment is needed.
Medical school and continuing education programs are now beginning to recognize this deficiency.
ECS modules are being incorporated into school curriculum by some, while professional organizations are developing guidelines for education about cannabis.
Dr. Broselid is acutely aware that bridging this education gap is crucial for improving personalized medicine and patient care within an evolving therapeutic landscape with increasing popularity for cannabis therapies.
Source: cannabishealthnews.co.uk
Cannabis Use and Physical Activity Levels

Findings of a recent analysis of Belgian Health Interview Survey data regarding physical activity indicated no difference for past-month cannabis users of 15-64 years compared with non-users.
This defies the stereotype that cannabis use causes a loss of motivation or being less physically active. The studies actually support that cannabis use does not impact athletes participating in sporting events.
The population-based sample, which included a representative sample of Belgian citizens, made use of precise data about patterns of cannabis use, and measures of physical activity.
The participants were screened for various areas of physical activity, including recreation, occupational, and transport activities.
The research showed that cannabis users were just as active as non-users for all categories assessed.
These findings contradict earlier assumptions that individuals who use cannabis are less motivated or less active.
The “couch-lock” stigma, commonly linked with cannabis use, is unproven when looking at actual patterns of behavior.
Researchers have a variety of theories to account for the findings, such as that cannabis may reduce exercise-related pain and inflammation, which would actually make exercise easier for some people.
The study further noted that a majority of users of cannabis had reported using the drug alongside exercise, particularly for leisure activities.
Those participating reported that cannabis increased liking for some activities, for instance, yoga, biking, or hiking.
However, experts caution that these findings do not necessarily justify pre-exercise use of cannabis, since safety issues and individual responses are extremely varied.
The research calls for more refined comprehension of cannabis impact on behavior and questions simplistic assumptions about users’ ways of life.
Source: pubmed.ncbi.nlm.nih.gov
Cannabis as an Opioid Alternative in Rheumatic Diseases

Because there is an opioid epidemic, alternative options are clearly needed for pain control. A review published in the Proceedings (Baylor University Medical Center) covers the use of cannabis as a potential treatment option for rheumatologic disease patients.
There are some studies demonstrating that cannabinoids are temporarily effective for symptom improvement of fibromyalgia, including mood and quality of sleep, there is no such evidence for rheumatoid arthritis.
The article reviewed a number of studies on cannabis use for a range of rheumatologic diseases with mixed results across different diseases.
In individuals with fibromyalgia, various studies indicated that pain, sleep, and overall quality of life all were better with cannabis-based medications.
For osteoarthritis and rheumatoid arthritis, however, the evidence was less strong, with a few studies reporting only slightly more improvement than with placebos.
The authors highlighted that there must be consideration of cannabis as part of a multimodal regimen for pain control, particularly among those with an insufficient response to conventional modalities or with side effects of opioid analgesic.
They stated that cannabinoids would probably provide certain benefits in managing the complex symptom profiles of rheumatologic illnesses, often entailing pain, insomnia, and mood disturbance.
Overall, there are safety issues, and there is a mention of potential side effects such as dizziness, dry mouth, and cognitive effects.
The authors emphasize the value of meticulous patient selection and monitoring with regard to cannabis therapeutics.
They suggest bigger controlled studies for further definition of ideal dosing, delivery, and long-term effect in rheumatologic disease populations because evidence up until now is biased by differences in methodology among studies and by limited sample size.
Source: pmc.ncbi.nlm.nih.gov
Cannabis Oil in Treating Parkinson’s Disease: A Case Report
A recent case published in the Brazilian Journal of Biology covers the use of cannabis oil in a 77-year-old man with severe Parkinson’s disease.
The patient displayed remarkable improvements in the motor functions, i.e., movement and reduced tremors, and non-motor signs, i.e., mood and speech.
These findings suggest that cannabis oil is a potential drug for Parkinson’s disease patients, and further research must be done to confirm its effectiveness and mode of action.
The patient suffered from clinically diagnosed Parkinson’s disease for several years and experienced worsening of his signs despite receiving standard treatments.
Soon after initiating cannabis oil therapy with a physician’s supervision, the patient showed incredible improvements overall.
The characteristic motor features of bradykinesia (slow movement), rigidity, and tremor were all relieved. Sleeping quality was better, there was reduced anxiety, and there were improvements in family interaction.
The treatment regimen included gradually titrating the doses of cannabis oil, with close monitoring of benefits and side effects.
The patient’s conventional Parkinson’s medications were also maintained throughout the period of treatment, so that cannabis oil is an adjuvant therapy, not a replacement for standard therapies.
The benefits were sustained over several months of follow-up, indicating advantages over the longer term.
The authors acknowledge the confines of individual case reports yet point out a potential significance for such findings with regards to Parkinson’s disease treatment.
They suggest that cannabinoids affect a number of neurochemical pathways targeted by Parkinson’s disease, with neuroprotective effects separate from those responsible for symptom control.
The paper suggests larger controlled trials to determine whether there is therapeutic potential for cannabis oil among Parkinson’s disease groups.
Source: scielo.br
Medical Cannabis for Chronic Pain
An article published by the Journal of Cannabis Research discussed medical cannabis effectiveness with regards to chronic pain and influencing factors.
The studies showed that the patients achieved notable pain relief, with males potentially receiving more benefits compared to women.
These observations support the importance of individualized approaches for medical cannabis treatments and imply a need for further studies for optimal patient responses.
The study entailed a thorough analysis of demographics among patients, pain dynamics, patterns of cannabis use, and reactions to treatment.
Data was collected on several variables such as age, sex, duration of pain, prior treatments, cannabis dose, and routes of administration.
The findings showed that while improvement in pain occurred among women and men, male participants reported greater improvements in pain score and function.
There were a number of theories put forth for explaining the gender differences that were seen, including differences in endocannabinoid function, differences in pain experience and reporting, and influences of hormonal effects.
The data also pinpointed some further predictors of a successful outcome, including initial pain severity, previous use of opioids, and the specific pain disorder being treated.
The research highlighted the difficulty of treating chronic pain and the importance of individualized treatment.
Factors such as cannabis strain selection, dosing regimens, and delivery all appeared to influence treatment outcomes.
The authors described that successful treatment with medical cannabis often required an adjustment and optimizing period, during which doctors and patients worked together toward finding the best approach.
Source: publications.sciences.ucf.edu